Kevin A. Day; Yen-Sheng Lin, MS; Michael Boninger, MD; Nathan Hogaboom, BS, Alicia M. Koontz, PhD, RET;
Department of Veterans Affairs, Human Engineering Research Laboratories, Pittsburgh, PA; Department of Rehabilitation Science and Technology, University of Pittsburgh, Pittsburgh, PA;
BACKGROUND
Subacromial impingement syndrome is reported as the most common reason for shoulder discomfort (van der Windt, 1995). Research has shown that shoulder discomfort due to subacromial impingement is associated with muscle fatigue (Wiker 1989) and shoulder dysfunction (Ludewig, 2000). The subacromial space consists of the humeral head, acromion, coracoacromial ligament, subacromial bursa, and the acromioclavicular joint (Neer, 1972). Subacromial impingement refers to the encroachment of the supraspinatus as a result of the subacromial space narrowing (Michener, 2003). Because of the high frequency in which manual wheelchair users (MWUs) perform weight bearing and repetitive upper-body activities, they are at an extremely high risk for developing shoulder pathology (Morrow, 2011). Recently, ultrasonography has been used as the preferred technique for evaluating the subacromial space (Azzoni, 2004) because of its portability, radiation-free, and non-invasive imaging. Acromiohumeral distance (AHD), the 2-D linear measurement between the most inferior aspect of the acromion and the humeral head (Cholewinski, 2007), is utilized as a statistically reliable way (ICC ≥ 0.90) to measure the subacromial space (Pijls, 2009). Therefore, AHD measures using ultrasound is a useful research tool for quantitatively evaluating the consequences of specific experimental interventions on the subacromial space.
The primary mechanism responsible for subacromial impingement is superior humeral migration (Chopp, 2012). The narrowing of the subacromial space is theorized to be caused by intrinsic and extrinsic factors (Michener, 2003). Intrinsic factors include tendon tears that occur due to degeneration of the tendon from long-term use (Budoff, 1998) whereas extrinsic factors include those that are a result of mechanical compression of structures surrounding the tendon due to mechanisms such as poor posture or altered glenohumeral kinematics (Neer, 1972). Superior humeral migration occurs in healthy individuals as the shoulder abducts from 0 to 90 degrees (Graichen, 1999). Within this range of shoulder motion, the upward force of the deltoid muscle overwhelms the stabilizing force of the rotator cuff muscles, thus resulting in a decrease in the AHD (Chopp, 2010). Because of this counterbalance relationship between the deltoid and rotator cuff muscles, investigators (Chopp, 2012) have studied the effects of rotator cuff muscle fatigue on the subacromial space. Muscle fatigue can be defined as a reduction in the ability of the muscle to generate force or power due to exercise (Enoka, 2008). Teyhen et al. reported that AHD narrowing increased following fatigue exercises regardless of the degree of shoulder abduction using digital fluoroscopy imaging techniques (Teyhen, 2008).
While past studies have evaluated the effects of varying degrees of shoulder abduction and muscle fatigue on the AHD (Graichen, 1999), no studies to our knowledge have investigated the effects of shoulder positions on the AHD following rotator cuff muscle fatigue in MWUs. The purpose of this study is to determine what positions are most sensitive to detecting changes in AHD following repeated upper extremity exercises. We hypothesize that MWUs will show a more statistically significant change in AHD. Additionally, we hypothesize that increased levels of shoulder abduction will be correlated to a lesser change in AHD following repeated upper extremity exercises.
METHODS
Participants
The study included 10 MWUs (2 tetraplegia and 8 paraplegia) as the case group (age: 35.0 ± 10.4; weight: 153.0 ± 55.0 lbs, height: 68.0 ± 4.9 inches) and 10 healthy, unimpaired individuals as the control group (age: 36.0 ± 11.5, weight: 175.0 ± 29.7 lbs, height: 69.0 ± 3.6 inches). Participants in the control and case group were recruited for this study on the basis that they were over 18 years of age, English speaking, and self-reported that they could complete multiple weight relief push-ups. Exclusion criteria included any history of fractures or dislocations in the shoulder, elbow and wrist from which the participant had not fully recovered, the presence of implants or pacemakers, any pain in an upper extremity that could interfere with normal function and activity, and a history of a cardiopulmonary condition that could be exacerbated. MWU were recruited for this study on the basis that they had a spinal cord injury over 1 year ago and used a manual wheelchair as their primary means for mobility. All participants provided an omni-pain scale reading at the beginning of the study to provide a baseline measurement. Written informed consent was signed by each subject prior to performing the procedure.
Ultrasound Imaging Protocol
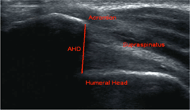 Figure 1. Acromiohumeral Distance (AHD) measured from the most inferior aspect of the acromion to the humeral head
Figure 1. Acromiohumeral Distance (AHD) measured from the most inferior aspect of the acromion to the humeral headAll ultrasound images were collected using a Philips HD11 1.0.6 ultrasound machine with a 5-12 MHz 50 mm linear array transducer (Philips Medical Systems, Bothell, WA). The subacromial space was evaluated by placing the transducer on the lateral surface of the shoulder and imaging along the longitudinal axis of the humerus. Acromiohumeral distance (AHD) was taken as the minimum distance from the inferior aspect of the acromion to the point of entry of the tendon into the acoustic shadow of the humeral head (Girometti, 2006) (Figure 1). Images were taken of the shoulder on the non-dominant side in 0, 45, and 90 degrees abduction in the scapular plane (Chopp, 2010). Further, the 45 and 90 degrees abduction were evaluated under active and passive conditions. A Biodex Isokinetic Dyanometer ™ (Biodex Medical Systems, Inc, Shirley, New York) was used to maintain the participant’s arm in the prescribed angle of elevation and provide isometric resistance for the active conditions (Figure 2). Participants were instructed to grab the handle of the Biodex with their arm internally rotated (Graichen, 1999).
Fatiguing Protocol
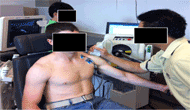 Figure 2. Participants maintained their arm at the prescribed angle of shoulder elevation by grabbing the handle bar of the Biodex. Ultrasound images were collected at 0, 45, and 90 degrees of shoulder abduction. These images are from a demonstration and not an actual participant.
Figure 2. Participants maintained their arm at the prescribed angle of shoulder elevation by grabbing the handle bar of the Biodex. Ultrasound images were collected at 0, 45, and 90 degrees of shoulder abduction. These images are from a demonstration and not an actual participant.Two exercises were used in this study to achieve rotator cuff muscle fatigue: weight relief pushups and external shoulder rotation exercises. The order of which the participant completed these exercises was randomized and the participant was given a thirty minute rest in between the two exercises to minimize the carry over effect. When completing the weight relief pushups, participants would start in a seated position and then extend their elbows. Participants were instructed to continue the exercise at one pushup per two seconds until they reported they could not complete any more pushups. For the external shoulder rotation exercises, the Biodex provided isokinetic resistance. The angular velocity was 60 degrees per second for external rotation and 180 degrees per second for internal rotation. The participants started with their non-dominant elbow at 90 degrees of flexion and shoulder at 0 degrees of rotation. They then externally rotated their shoulder 45 degrees against the isokinetic force and repeated that exercise until they reported they could not do any more. Following completion of each exercise, the participants provided a Borg scale and omni-pain scale reading. Research shows that self-reported exertion levels are closely related to EMG signs of fatigue (Hummel, 2005). Similar to the protocol used by Chopp et al (Chopp 2010), a Borg scale reading of 10 or over was necessary to confirm muscle fatigue and move on to post-fatigue imaging.
Statistical Analysis
Interclass correlation coefficients (ICC) were used to evaluate the inter- and intra-rater reliability of AHD measures. A 2 X 2 mixed-design analysis of variance (ANOVA) was used to analyze AHD at the three angles of shoulder elevation (0, 45, and 90 degrees) within subjects in pre- and post-fatigue conditions as well as between subjects for both subject populations. The level of significance was set at 0.05. Standard error of measurement and minimum detectable difference were calculated to detect a true AHD change that significantly exceeded the measurement error (Leong, 2011). All data analysis was performed using SPSS (version 20.0, SPSS Inc, Chicago, IL).
RESULTS
Reliability testing for using ultrasound as an imaging technique to evaluate AHD for the control group revealed an ICC of 0.807 to 0.928 intra-rater reliability for two independent evaluators and an ICC of 0.926 for inter-rater reliability. For the case group, an ICC of 0.903 and 0.841 was found for inter-rater and intra-rater reliability respectively, thus confirming the high reliability of ultrasonography when used to image the subacromial space. Descriptive data of the change in AHD before and after fatigue for each subject population is shown in Table 1.
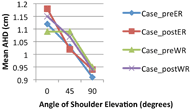
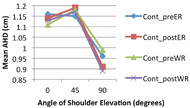 Figure 4. Acromiohumeral distance for the control group at varying degrees of shoulder abduction.
Figure 4. Acromiohumeral distance for the control group at varying degrees of shoulder abduction. When comparing within-subject effects, AHD was reduced at 90 degrees of abduction under active conditions (p=0.028) for both the case and control groups. In addition, a trend of increased AHD was found at 0 degrees of abduction for the weight relief fatiguing exercises (p=0.083). There was no significant difference found between the case group and the control group with respect to change in AHD due to fatigue.
Figures 3 and 4 display the effects of the angle of shoulder abduction on the mean AHD for MWUs and healthy individuals, respectively, for both external rotation and weight relief pushup exercises. MWUs experienced a continued decrease in AHD from 0 to 45 to 90 degrees of shoulder abduction (Figure 3). Healthy individuals, however, displayed a pattern in which mean AHD increased from 0 to 45 degrees and then decreased from 45 to 90 degrees of shoulder abduction. The minimal detectable difference was found to be approximately 0.13 cm for the control group.
DISCUSSION
The results show that there is no statistically significant difference in the effects that fatigue has on AHD when comparing MWUs to healthy individuals. Our results agree in part with those from previous studies in which fatiguing exercise results in a decrease in AHD (Graichen, 1999). AHD was decreased when the shoulder was held at 90 degrees of abduction post fatigue but was slightly larger when the shoulder was held passively at 0 degrees. Shoulder muscles used to keep the glenohumeral joint stable at 90 degrees may have become fatigued resulting in the compressed space. This finding points to the potential danger of impingement when performing repetitive overhead shoulder activities.
In fatigued shoulders, the AHD tends to reduce continuously from 0 to 90 degrees of abduction (Graichen, 1999). From looking at Figures 3, 4 and Table 1, this pattern was confirmed for the most part. The apparent increase in mean AHD from 0 to 45 degrees of abduction in healthy individuals (Figure 4) compared to that found in the wheelchair user group although not statistically different may provide insight into the pathokinetics of the wheelchair users’ shoulders. Both groups were similar in age and size, however a majority of wheelchair users experience early degenerative changes in the shoulder that predispose them to shoulder problems due to overuse (Lal, 1998). Thus ‘healthy’ shoulders may have a protective mechanism (e.g. kinematic pattern) that keeps the space intact through arm abduction. For example, other factors such as scapular orientation, trunk posture, acromial shape, and tendon deterioration can all affect the subacromial space (Chopp, 2010). Many high force wheelchair activities occur within the 45 to 60 degree ranges of shoulder abduction (e.g. propulsion and transfers) which may increase wheelchair users’ risk for shoulder pain and injuries. It would be beneficial for further studies to examine other factors responsible for narrowing of the space.
Muscle fatigue was not objectively confirmed in this study so it is possible that some people were limited by pain or discomfort in performing the activities rather than fatigue. The fatigued state of the infraspinatus muscle of the rotator cuff can limit the stabilizing force and result in encroachment of the humeral head into the space (Chopp, 2012). Future research is needed to confirm infraspinatus fatigue using EMG. Further research should also focus on limiting the confounding factors present when evaluating the subacromial space. Kinematics should be recorded on the trunk, scapula, and humerus to track the 3-D movement during the fatiguing and imaging protocols.
CONCLUSION
Ultrasonography proved a reliable means to evaluate the subacromial space and measure the AHD. Shoulders actively positioned in a 90 degree abducted posture showed narrowing of the AHD following rotator cuff fatiguing exercise. AHD consistently narrowed throughout the range of shoulder abduction movement in manual wheelchair users. Our findings provide insight into the mechanisms of shoulder impingement. Future studies are recommended to evaluate the relationship between subacromial space narrowing and other activities of daily living like wheelchair transfers, wheelchair propulsion, and overhead activities.
Subject Population |
Fatiguing Exercisea |
Shoulder Abduction Angle |
Pre-Exerciseb |
Post-Exerciseb |
Case |
ER |
0° |
1.12 ± 0.14 |
1.18 ± 0.20 |
45° Active |
0.93 ± 0.22 |
0.93 ± 0.24 |
||
45° Passive |
1.03 ± 0.20 |
1.02 ± 0.25 |
||
90° Active |
0.88 ± 0.20* |
0.82± 0.19* |
||
90° Passive |
0.91 ± 0.22 |
0.94 ± 0.23 |
||
WR |
0° |
1.09 ± 0.14^ |
1.15 ± 0.15^ |
|
45° Active |
0.96 ± 0.21 |
0.96 ± 0.20 |
||
45° Passive |
1.09 ± 0.15 |
1.07 ± 0.16 |
||
90° Active |
.89 ± 0.23 |
0.86 ± 0.22 |
||
90° Passive |
0.95 ± 0.25 |
0.94 ± 0.24 |
||
Control |
ER |
0° |
1.16 ± 0.16 |
1.14 ± 0.16 |
45° Active |
0.95 ± 0.28 |
1.02 ± 0.19 |
||
45° Passive |
1.15 ± 0.22 |
1.19 ± 0.21 |
||
90° Active |
0.84 ± 0.11* |
0.79 ± 0.12* |
||
90° Passive |
0.96 ± 0.17 |
0.91 ± 0.22 |
||
WR |
0° |
1.11 ± 0.21^ |
1.13 ± 0.17^ |
|
45° Active |
0.92 ± 0.24 |
0.92 ± 0.17 |
||
45° Passive |
1.18 ± 0.22 |
1.17 ± 0.22 |
||
90° Active |
0.86 ± 0.17 |
0.83 ± 0.13 |
||
90° Passive |
0.99 ± 0.21 |
0.89 ± 0.18 |
||
|
||||
REFERENCES
Azzoni R, Cabitza P, & Parrini M (2004). Sonographic evaluation of subacromial space. Ultrasonics, 42, 683.
Budoff JE, Nirschl RP, & Guidi EJ (1998). Debridement of partial-thickness tears of the rotator cuff without acromioplasty. Long-term follow-up and review of the literature. J. Bone Joint Surg. Am, 80, 733-748.
Cholewinski JJ, Kusz DJ, Wojciechowski P, Cielinski LS, & Zoladz MP (2007). Ultrasound measurement of rotator cuff thickness and acromio-humeral distance in the diagnosis of subacromial impingement syndrome of the shoulder. Knee Surg Sports Traumatol Arthrosc, 16, 408.
Chopp JN, & Dickerson CR (2012). Resolving the contributions of fatigue-induced humeral migration and scapular reorientation on the subacromial space: An orthopaedic geometric simulation analysis. Human Movement Science, 1-13.
Chopp JN, O’Neill JM, Hurley K, & Dickerson CR (2010). Superior humeral head migration occurs after a protocol designed to fatigue the rotator cuff: A radiographic analysis. J Shoulder Elbow Surg, 19, 1137-1144.
Enoka RM, & Duchateau J (2008). Muscle fatigue: what, why and how it influences muscle function. J Physiol, 586, 11-23.
Girometti R et al (2006). Supraspinatus tendon US morphology in basketball players: correlation with main pathologic models or secondary impingement syndrome in young over-head athletes. Radiol Med, 111,42.
Graichen H et al (1999). Subacromial space width changes during abduction and rotation- a 3-D MR imaging study. Surg Radiol Anat, 21, 59-64.
Hummel A et al. (2005). Relationship between perceived exertion and mean power frequency of the EMG signal from the upper trapezius muscle during isometric shoulder elevation. Eur J Appl Physiol, 95, 321-326.
Lal S (1998). Premature degenerative shoulder changes in spinal cord injury patients. Spinal Cord, 36(3), 186-89.
Leong HT, Tsui S, Ying M, Leung VY, & Fu SN (2011). Ultrasound measurements on acromio-humeral distance and supraspinatus tendon thickness: Test-retest reliability and correlations with shoulder rotational strengths. Journal of Science and Medicine in Sport, 670.
Lin YS, Koontz A, Worobey L, & Boninger M (2012). Effect of muscle fatiguing tasks on subacromial space in manual wheelchair users. RESNA
Ludewig PM, & Cook TM (2000). Alterations in shoulder kinematics and associated muscle activity in people with symptoms of shoulder impingement. Phys. Ther, 80(3), 276-291.
Michener LA, McClure PW, & Karduna AR (2003). Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clinical Biomechanics, 18(5), 369-379.
Morrow MM, Kaufman KR, & An KN (2011). Scapula kinetics and associated impingement risk in manual wheelchair users during propulsion and weight relief lift. Clin. Biomech, 4, 352-357.
Neer CS (1972). Anterior acromioplasty for the chromic impingement syndrome in the shoulder: a preliminary report. J. Bone Joint Surg. [Am], 54, 41-50.
Pijls BG, Kok FP, Penning LIF, Guldemond NA, & Arnes HJ (2009). Reliability study of the sonographic measurement of the acomiohumeral distance in symptomatic patients. Journal of Clinical Ultrasound, 38(3), 128-134.
Teyhen DS, Miller JM, Middag TR, & Kane EJ (2008). Rotator cuff fatigue and glenohumeral kinematics in participants without shoulder dysfunction. Journal of Athletic Training, 43(4), 352-358.
van der Windt DA, Koes BW, & de Jong BA (2000). Shoulder disorders in general practice: Incidence, patient characteristics, and management. Ann Rheum Dis, 54, 959-964.
Wiker SF, Chaffin DB, & Langolf GD (1989). Shoulder posture and localized muscle fatigue and discomfort. Ergonomics, 32, 211-237.
ACKNOWLEDGEMENTS
This material is based upon work supported by the Department of Veterans Affairs Rehabilitation Research and Development Service (Project Number: B6789C) as well as the ASPIRE program (NSF Grant Number: 0849878).
Thank you to the Human Engineering Research Laboratories where the work for this study was performed.
The contents do not represent the views of the Department of Veterans Affairs or the United States Government.